For patients experiencing atrial fibrillation, Sotalol often serves as a cornerstone in treatment plans. This antiarrhythmic medication plays a significant role in managing heart rhythms, providing a reliable method to restore and maintain normal sinus rhythm. Administering Sotalol requires careful monitoring, especially in those with underlying cardiac conditions.
When prescribing Sotalol, it is vital to initiate treatment under close supervision. Start with a low dose to gauge tolerance, adjusting as appropriate based on kidney function and QT interval on EKG. Regular follow-ups are crucial in assessing the drug’s efficacy and ensuring that side effects, like bradycardia or hypotension, are managed promptly.
Sotalol not only aids in rhythm control but can also be effective in preventing the recurrence of atrial fibrillation. Many clinicians recommend pairing Sotalol with additional therapies, such as anticoagulants, to mitigate the risk of stroke associated with the condition. Monitoring electrolyte levels and kidney function remains a priority throughout the treatment duration.
By providing a structured approach to Sotalol administration in patients with atrial fibrillation, healthcare providers can enhance patient outcomes and improve quality of life. Open communication about potential side effects and the importance of adherence to prescribed regimens is fundamental in empowering patients in their treatment journey.
- Understanding Sotalol in the Management of Atrial Fibrillation
- Mechanism of Action: How Sotalol Affects Atrial Fibrillation
- Dosage and Administration: Guidelines for Sotalol in AF Patients
- Monitoring and Managing Side Effects of Sotalol Therapy
- Common Side Effects
- Management Strategies
- Clinical Outcomes: Efficacy of Sotalol in Atrial Fibrillation Cases
- Reduction of Hospitalization Rates
- Improvement in Quality of Life
Understanding Sotalol in the Management of Atrial Fibrillation
Sotalol serves as a key option in managing atrial fibrillation (AF) by offering both rate control and rhythm management. This medication is classified as a Class III antiarrhythmic drug, primarily affecting potassium channels while also exhibiting beta-blocking properties.
For optimal use, healthcare providers typically initiate sotalol treatment in a controlled environment, monitoring patients closely during the first few doses due to the potential for significant QT interval prolongation. Regular ECG assessments are essential during therapy to ensure safety.
- Dosing: The usual starting dose for sotalol is 80 mg taken orally twice daily, which can be adjusted based on tolerance and the patient’s renal function. In patients with adequate renal function, the dose can be titrated to a maximum of 320 mg per day.
- Monitoring: Continuous or frequent ECG monitoring is recommended during initiation and dosage adjustments. Monitoring electrolytes, particularly potassium and magnesium, is also crucial, as imbalances can exacerbate the risk of arrhythmias.
- Side Effects: Common side effects include fatigue, dizziness, and bradycardia. Patients with a history of asthma or chronic obstructive pulmonary disease should use caution, as beta-blockade can worsen respiratory conditions.
When considering sotalol, evaluate the risk of proarrhythmia, particularly in patients with a high baseline QT interval or other risk factors, such as concurrent use of drugs that prolong QT interval.
- Patient Selection: Ideal candidates for sotalol treatment typically have paroxysmal or persistent AF where rhythm control is a priority.
- Long-term Management: Sotalol can help maintain sinus rhythm post-conversion, supporting better long-term outcomes in selected populations.
- Discontinuation: Gradual tapering of sotalol is advisable to prevent rebound tachycardia or exacerbation of AF upon cessation.
Patient education plays a significant role in effectively managing atrial fibrillation with sotalol. Inform patients about potential side effects and the importance of adherence to scheduled follow-up visits for monitoring. By doing so, healthcare providers can enhance the therapeutic outcomes of sotalol therapy in managing atrial fibrillation.
Mechanism of Action: How Sotalol Affects Atrial Fibrillation
Sotalol primarily acts as a Class III antiarrhythmic agent. It blocks potassium channels, slowing the repolarization of cardiac action potentials. This action extends the refractory period, which helps control heart rhythm during atrial fibrillation.
By inhibiting rapid potassium currents, Sotalol increases the duration of the action potential and the refractory period in the atria. This modulation of electrical activity reduces the likelihood of reentrant circuits that contribute to atrial fibrillation.
In addition to its potassium channel-blocking effects, Sotalol also exhibits beta-adrenergic blockade. This contributes to a decrease in heart rate and reduces sympathetic stimulation, which can provoke arrhythmias. Through these dual mechanisms, Sotalol stabilizes the electrical activity in the atria.
Clinical studies demonstrate that Sotalol significantly decreases the frequency of atrial fibrillation episodes. This effect is particularly beneficial for patients with persistent or recurrent atrial fibrillation who require effective long-term management.
Monitoring renal function is crucial during Sotalol therapy, as impaired renal clearance can lead to increased drug levels and a higher risk of side effects. Dose adjustments may be necessary based on renal function to ensure patient safety and optimal therapeutic outcomes.
Overall, Sotalol’s unique mechanism of action helps manage atrial fibrillation effectively, promoting a more stable heart rhythm and improving patients’ quality of life.
Dosage and Administration: Guidelines for Sotalol in AF Patients
The typical oral starting dose of sotalol for atrial fibrillation (AF) is 80 mg to 120 mg taken twice daily. Adjustments may be necessary based on patient response and tolerance. Monitor patients closely during the initiation phase due to the risk of potential adverse effects such as bradycardia or hypotension.
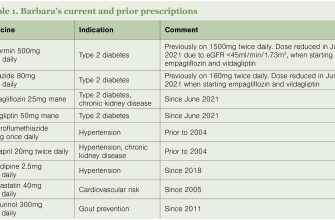
For patients with renal impairment, consider dose adjustments. In those with a creatinine clearance below 60 mL/min, reduce the dose or increase the dosing interval to prevent accumulation and toxicity. A common approach is to administer doses at 24-hour intervals rather than every 12 hours.
Assess the QT interval before starting therapy and periodically during treatment. Sotalol can prolong the QT interval, increasing the risk of torsades de pointes. Regular ECG monitoring during dose adjustments or upon experiencing symptoms of arrhythmia is essential.
During the first few days of therapy, conduct inpatient monitoring for those on higher doses or with significant comorbidities. This close observation aids in catching any serious side effects early.
Instruct patients to take sotalol consistently, with or without food, to maintain stable plasma levels. Avoid abrupt discontinuation to reduce the risk of rebound tachyarrhythmia.
Reassess the need for continued therapy every three to six months, considering both efficacy in maintaining sinus rhythm and the occurrence of side effects. Engage patients in discussions about their treatment goals and any concerns they may have regarding their medication.
Monitoring and Managing Side Effects of Sotalol Therapy
Regular monitoring of heart rate and rhythm is crucial while on Sotalol therapy. Patients should undergo periodic ECG evaluations to assess QT interval prolongation, which can increase the risk of torsades de pointes. Adjustments to dosage may be needed based on these readings.
Common Side Effects
Fatigue, dizziness, and bradycardia are frequently reported. Encourage patients to report any significant changes in energy levels or unusual heart rhythms. Educate your patients about recognizing symptoms such as excessive fatigue, weakness, or fainting, which can indicate bradycardia.
Management Strategies
For patients experiencing side effects, consider dose adjustment or transitioning to alternative therapies if symptoms do not resolve. Regular follow-ups, including blood pressure assessments, can help in early identification of issues. Advise patients on lifestyle modifications, including hydration and balanced nutrition, to support overall heart health during therapy.
Clinical Outcomes: Efficacy of Sotalol in Atrial Fibrillation Cases
Sotalol significantly reduces the incidence of recurrent atrial fibrillation (AF), providing an effective option for long-term rhythm control. Clinical studies demonstrate that sotalol achieves a maintenance of sinus rhythm in approximately 50-70% of patients after one year of treatment. Dosage adjustments based on renal function and patient tolerance enhance outcomes while minimizing side effects.
Reduction of Hospitalization Rates
Patients under sotalol treatment typically experience fewer hospitalizations due to AF-related complications. Data indicates a reduction in emergency room visits and inpatient stays, highlighting sotalol’s role in improving patient stability. Surveillance programs show that consistent monitoring and appropriate dose adjustments contribute to maintaining rhythm control, thereby reducing healthcare burdens.
Improvement in Quality of Life
Long-term sotalol therapy correlates with enhancements in quality of life metrics. Patients report reduced symptoms associated with AF, such as palpitations and fatigue. This improvement is measured through validated questionnaires, demonstrating favorable outcomes in daily functioning and overall well-being. Continual follow-up and patient education on managing their condition lead to improved adherence to treatment regimens.