Yes, lisinopril can impact kidney function, particularly in certain populations. Regular monitoring of kidney function is advisable for patients taking this medication, especially those with pre-existing kidney conditions or diabetes. Medical professionals recommend routine blood tests to assess creatinine levels and the estimated glomerular filtration rate (eGFR) during treatment.
Patients may experience changes in kidney performance as lisinopril affects blood flow to the kidneys. This alteration can lead to temporary increases in serum creatinine levels. It’s important to consult a healthcare provider if significant changes occur or if symptoms like swelling, weight gain, or urine changes arise.
While lisinopril is generally well-tolerated, individuals should not dismiss any unusual symptoms. Staying in touch with a healthcare professional and adhering to prescribed follow-ups ensure safety while using this medication. Keeping a close watch on blood pressure levels and overall kidney health can help manage any potential risks effectively.
- Does Lisinopril Cause Kidney Problems?
- Understanding Lisinopril and Its Uses
- Key Uses of Lisinopril
- Possible Side Effects and Kidney Health
- How Lisinopril Affects Kidney Function
- Potential Effects on Kidney Health
- Recommendations for Patients
- Identifying the Signs of Kidney Issues While on Lisinopril
- Risk Factors for Kidney Problems in Lisinopril Users
- Recommendations for Monitoring Kidney Health During Treatment
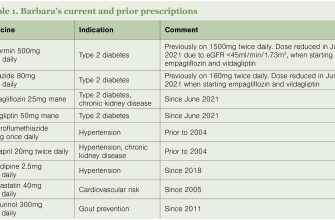
- Medication Review
- Monitor Blood Pressure
- Alternative Medications and Their Kidney Safety
Does Lisinopril Cause Kidney Problems?
Yes, lisinopril can impact kidney function, but its effects vary among individuals. Regular monitoring of kidney health is advisable for anyone taking this medication.
The following points highlight the relationship between lisinopril and kidney health:
- Lisinopril is an ACE inhibitor commonly prescribed for hypertension and heart failure.
- This medication may cause a temporary increase in serum creatinine levels, indicating stress on the kidneys.
- Patients with pre-existing kidney conditions or dehydration are at higher risk for adverse effects.
- Taking diclofenac or other nonsteroidal anti-inflammatory drugs (NSAIDs) alongside lisinopril can further strain kidney function.
- Signs of potential kidney issues include a decrease in urine output, swelling in extremities, and fatigue.
Healthcare providers typically recommend routine blood tests to monitor kidney function while on lisinopril. Adjustments to dosage or alternative medications may be necessary based on these assessments.
If you experience unusual symptoms or have concerns about your kidney health while taking lisinopril, consult your doctor for personalized advice and management options.
Understanding Lisinopril and Its Uses
Lisinopril helps manage hypertension and heart failure by relaxing blood vessels, allowing blood to flow more easily. This medication is an ACE inhibitor, which blocks the action of a substance in the body that narrows blood vessels. As a result, individuals often experience lower blood pressure and decreased workload on the heart.
Key Uses of Lisinopril
Initially approved for treating high blood pressure, lisinopril has established itself in other areas, such as:
- Heart failure management, aiding in reducing symptoms and improving quality of life.
- Post-myocardial infarction treatment, helping to prevent further heart complications.
- Kidney protection for patients with diabetes, as it can reduce the progression of diabetic nephropathy.
Possible Side Effects and Kidney Health
While lisinopril is beneficial for many, it can lead to side effects, including potential kidney issues. Regular monitoring of kidney function is crucial for those on this medication. Common side effects related to kidney health include:
| Side Effect | Description |
|---|---|
| Increased Blood Urea Nitrogen (BUN) | May indicate kidney strain; regular checks help manage levels. |
| Elevated Serum Creatinine | Reflects kidney function; monitoring is vital to prevent complications. |
Consult a healthcare provider if any unusual symptoms arise, ensuring kidney function remains stable throughout the treatment with lisinopril.
How Lisinopril Affects Kidney Function
Lisinopril can influence kidney function, particularly in individuals with pre-existing conditions. This medication, primarily used to manage hypertension and heart failure, can either maintain or compromise kidney health based on individual health status. Routine monitoring of kidney function through blood tests, specifically serum creatinine and potassium levels, is advisable for patients taking lisinopril.
Potential Effects on Kidney Health
In some cases, lisinopril may cause an increase in serum creatinine levels shortly after starting treatment. This effect is usually temporary and does not indicate permanent damage. Providers may adjust the dosage based on these readings. Lisinopril’s mechanism of action, primarily as an ACE inhibitor, can lead to renal artery dilation, which generally benefits kidney function but could pose risks when blood flow to the kidneys is already compromised.
Recommendations for Patients
If you have a history of kidney issues, discuss your medication regimen with your healthcare provider. Staying well-hydrated and monitoring blood pressure can support kidney health. Avoiding NSAIDs while on lisinopril is wise, as they can further strain the kidneys. Regular follow-up appointments will help ensure proper kidney function and adjust medications as needed.
Identifying the Signs of Kidney Issues While on Lisinopril
Monitor your body for specific signs indicating potential kidney issues while taking lisinopril. These signs may include:
Decreased Urine Output: Notice if you experience a significant reduction in urination. This can signal that your kidneys are not functioning properly.
Swelling: Observe any new swelling in your legs, ankles, or face. Accumulation of fluids can indicate kidney problems.
Fatigue: Unusual tiredness or weakness can arise from kidney dysfunction, as your body may not effectively filter toxins.
Nausea or Vomiting: Feelings of nausea or episodes of vomiting without an obvious cause may suggest kidney distress.
High Blood Pressure: Keep track of your blood pressure readings; kidney issues can lead to fluctuations. Report any significantly high readings to your healthcare provider.
Changes in Appetite: An unexplained loss of appetite can stem from issues with kidney function.
If you notice any of these symptoms, consult your healthcare provider immediately for assessment and potential adjustment of your medication. Regular monitoring through blood tests and urine tests can help ensure your kidneys remain healthy while on lisinopril.
Risk Factors for Kidney Problems in Lisinopril Users
Individuals taking lisinopril should be aware of specific risk factors that may contribute to kidney issues. Recognizing these factors helps in monitoring kidney function effectively.
- Pre-existing Kidney Disease: Those with chronic kidney disease (CKD) are at a higher risk of complications. Regular kidney function tests are crucial for this group.
- Dehydration: Inadequate fluid intake can strain the kidneys. Maintaining proper hydration is essential, especially during illness or extreme temperatures.
- Age: Older adults often have reduced kidney function. Close monitoring of renal function is advisable for this demographic.
- Diabetes: Diabetic patients face an increased risk of kidney damage. Blood sugar levels should be well-controlled to minimize risks.
- Heart Conditions: Individuals with heart disease may experience worsened kidney function. Regular check-ups can help manage both heart and kidney health.
- Concurrent Medications: Certain medications, including NSAIDs and diuretics, can negatively impact kidney function. Discuss all medications with your healthcare provider.
- Hypertension: High blood pressure itself can damage kidneys. Consistent monitoring and control of blood pressure are important steps for protection.
- High Protein Diet: Excessive protein can increase the workload on kidneys. A balanced diet is recommended for individuals on lisinopril.
Regular communication with healthcare providers is vital for anyone using lisinopril, especially if they identify with any of these risk factors. Taking proactive measures can significantly contribute to maintaining kidney health.
Recommendations for Monitoring Kidney Health During Treatment
Regular blood tests are critical. Schedule routine assessments of serum creatinine and blood urea nitrogen (BUN) levels to track kidney function. These tests help identify any changes early, allowing for timely interventions if necessary.
Stay hydrated to support kidney health, but be mindful of fluid intake if your healthcare provider advises limits. Monitor your weight consistently to catch any sudden increases that could indicate fluid retention, a possible side effect of medication.
Medication Review
Discuss all medications with your healthcare provider, including over-the-counter drugs and supplements. Some may affect kidney function or interact with lisinopril. Adjustments may be needed based on your overall health and kidney status.
Monitor Blood Pressure
Keep a close eye on your blood pressure at home. Maintaining your blood pressure within the target range is essential and can prevent additional strain on your kidneys. Use a reliable monitor and record your readings to share with your healthcare provider.
Alternative Medications and Their Kidney Safety
Angiotensin receptor blockers (ARBs), such as losartan and valsartan, serve as effective alternatives to lisinopril. Studies show they generally have a favorable kidney safety profile and are well-tolerated in patients with hypertension and heart failure. Monitoring kidney function remains important when using ARBs, but they often present fewer risks than ACE inhibitors.
Calcium channel blockers like amlodipine also provide a kidney-safe option. They work differently by relaxing blood vessels, leading to lower blood pressure. Research indicates minimal adverse effects on renal function, making them suitable for patients concerned about kidney issues.
Thiazide diuretics, including hydrochlorothiazide, can be considered as another alternative. These medications help reduce blood pressure while promoting sodium and water excretion. Although diuretics can occasionally lead to dehydration and electrolyte imbalances, they generally do not pose significant risks to kidney health when used properly.
Beta-blockers, such as metoprolol and atenolol, are effective for controlling blood pressure and reducing heart rate. They tend to be safe for kidneys, but renal function should be monitored, especially in patients with prior kidney concerns. Adequate hydration and regular follow-ups can mitigate potential risks.
Non-pharmacological options also deserve attention. Lifestyle changes, including a balanced diet and regular exercise, support kidney health and can enhance the effectiveness of any medication regimen. Education on diet modifications, especially sodium and protein intake, contributes positively to managing both blood pressure and kidney function.
Always consult healthcare providers when considering alternative medications. Individual health profiles, current treatments, and kidney function tests are crucial for determining the most suitable options. Regular monitoring and open communication with medical professionals lead to the best outcomes in managing blood pressure while sustaining kidney wellness.