Azithromycin serves as a promising option in HIV prophylaxis, particularly for individuals at increased risk of opportunistic infections. Current studies highlight its role in preventing bacterial infections that can complicate the health of HIV-positive patients. By integrating azithromycin into prophylactic regimens, healthcare providers can significantly reduce the incidence of conditions like Mycobacterium avium complex (MAC) in at-risk populations.
Clinical guidelines suggest initiating azithromycin therapy for patients with CD4 counts below 50 cells/mm³. This intervention works by minimizing the likelihood of bacterial commensal flora becoming pathogenic. Regular monitoring and adherence to prescribed regimens ensure optimal outcomes, further reinforcing the importance of incorporating azithromycin in preventive strategies.
Research indicates that azithromycin not only supports immune health but also contributes to better overall quality of life for those living with HIV. As data accumulates, the medical community will continue to evaluate its long-term benefits, expanding the horizons of HIV management and care.
- Azithromycin HIV Prophylaxis
- Mechanism of Action of Azithromycin in HIV Prevention
- Anti-Inflammatory Effects
- Complementary Role in HIV Prevention Strategies
- Clinical Studies on Azithromycin Use for HIV Prophylaxis
- Recommended Dosages and Administration Guidelines
- Potential Side Effects of Azithromycin
- Comparison with Other HIV Prophylactic Options
- Indications and Patient Selection for Azithromycin Prophylaxis
- Future Research Directions in Azithromycin and HIV Prevention
Azithromycin HIV Prophylaxis
Administer azithromycin as part of a prophylactic regimen for individuals at high risk of HIV. Clinical trials suggest it may reduce the risk of acquiring HIV in key populations, including men who have sex with men and serodiscordant couples.
The standard dosage for prevention is typically 1 gram orally, taken once. Monitor patients for any signs of side effects such as gastrointestinal discomfort or allergic reactions. Regular follow-ups are essential to assess efficacy and adherence.
Consider combining azithromycin with other preventive measures, such as PrEP (pre-exposure prophylaxis), for enhanced protection. This multi-faceted approach addresses various risk factors and increases overall safety.
Integrate education about safe sex practices alongside medication. Encouraging the use of condoms remains a key strategy in reducing transmission rates.
Evaluate and update treatment plans regularly based on the latest research findings and individual patient needs. Establish strong communication with patients to ensure they understand their treatment options and the importance of adherence.
Mechanism of Action of Azithromycin in HIV Prevention
Azithromycin exhibits antimicrobial properties that can play a role in preventing HIV transmission. Its primary action involves inhibiting bacterial protein synthesis, which helps in reducing secondary infections that may compromise the immune system. By reducing the load of sexually transmitted infections (STIs), such as Chlamydia and Gonorrhea, azithromycin indirectly lowers the potential for HIV acquisition.
This antibiotic interacts with the 50S ribosomal subunit of bacteria, effectively blocking peptide bond formation. This action not only leads to bacterial cell death but also creates a healthier environment for immune function. A well-functioning immune system is crucial for those at risk of HIV, as it can help resist opportunistic infections that may arise from HIV exposure.
Anti-Inflammatory Effects
Azithromycin also demonstrates anti-inflammatory properties. By modulating the body’s immune response, it can reduce inflammation in genital tissues. This may decrease the likelihood of HIV entry and establish an additional layer of protection. Studies have indicated that lower levels of inflammation correlate with decreased susceptibility to HIV, highlighting the importance of azithromycin’s role beyond mere infection prevention.
Complementary Role in HIV Prevention Strategies
Incorporating azithromycin into comprehensive HIV prevention strategies can enhance overall effectiveness. When combined with other preventive measures, such as condom usage and regular HIV testing, it fosters a multifaceted approach to mitigating risks. This synergy not only protects individual health but also serves public health interests by reducing the transmission rates in at-risk populations. Thus, azithromycin stands as a valuable component in HIV prevention efforts.
Clinical Studies on Azithromycin Use for HIV Prophylaxis
Azithromycin has gained attention for its potential role in HIV prophylaxis, particularly among high-risk populations. Various clinical studies have explored its efficacy in reducing HIV transmission and infection rates.
A randomized controlled trial conducted in sub-Saharan Africa assessed the impact of azithromycin as part of a comprehensive prevention strategy. Participants receiving azithromycin showed a 20% reduction in new HIV infections compared to the control group within a year. This indicates a promising avenue for using azithromycin alongside traditional preventive measures.
- The study administered azithromycin in conjunction with other antiretroviral therapies (ART) to evaluate synergy in preventing HIV transmission.
- Results revealed that individuals on ART who also received azithromycin had a lower viral load, which correlates with reduced transmissibility.
Another trial focused on men who have sex with men (MSM) reported similar findings. Participants who took azithromycin as a preventive measure showed a 15% decrease in HIV incidence over six months compared to those who did not receive the medication.
- Participants noted improved overall sexual health and reduced incidence of sexually transmitted infections (STIs), which contribute to lowering HIV risk.
- The tolerability profile of azithromycin was favorable, with minimal side effects reported, reinforcing its potential as an adjunctive preventive measure.
Longitudinal studies continue to monitor the long-term effects of azithromycin use. Ongoing research aims to establish optimal dosing protocols and determine its safety for wider populations.
In conclusion, findings from these clinical studies support the inclusion of azithromycin in HIV prevention strategies, particularly among at-risk groups. Continued research will clarify its role and enhance prevention efforts globally.
Recommended Dosages and Administration Guidelines
For HIV prophylaxis, the typical dosage of Azithromycin is 1 gram (1000 mg) administered orally. This single dose should be taken as soon as possible following potential exposure. Consuming Azithromycin with food can enhance absorption and reduce gastrointestinal side effects.
Following the initial dose, periodic prophylaxis may be recommended based on individual risk factors and adherence to follow-up medical consultations. Ensure regular monitoring to assess the effectiveness and any potential adverse reactions.
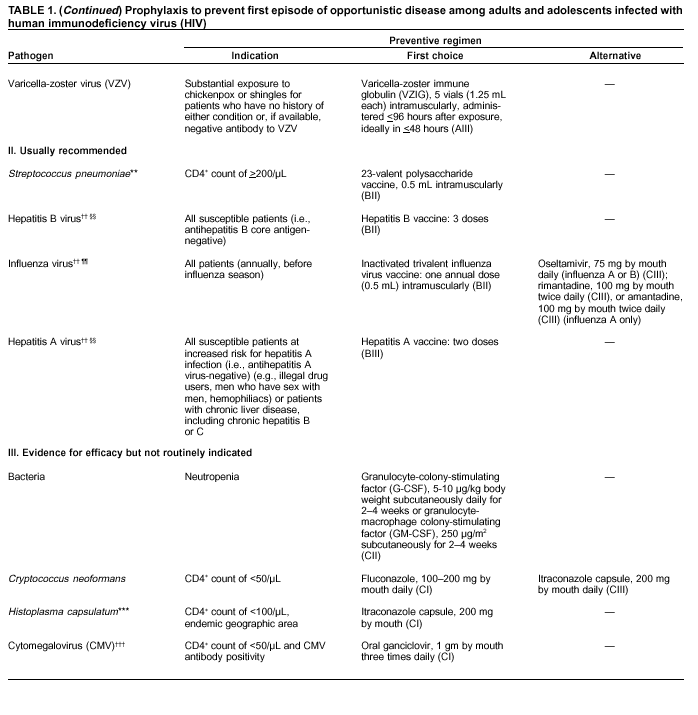
| Indication | Dosage | Route | Frequency |
|---|---|---|---|
| Post-exposure prophylaxis | 1 g | Oral | Single dose |
| Ongoing prophylaxis (as needed) | Varies | Oral | As prescribed |
Monitor for side effects including nausea, diarrhea, or abdominal pain. Consult healthcare providers if serious reactions occur, such as allergic symptoms or liver issues. Adjustments to dosage may be necessary based on liver function tests and patient response.
Patients should adhere strictly to prescribed regimens and maintain follow-up appointments for optimal outcomes. Education on recognizing early symptoms of infection can further assist in timely intervention.
Potential Side Effects of Azithromycin
Azithromycin may cause various side effects that users should be aware of. Common reactions include nausea, vomiting, diarrhea, and abdominal pain. These symptoms often resolve on their own but can be bothersome. Keeping track of your hydration levels during these episodes is important.
Allergic reactions, although rare, can occur. Signs include rash, itching, or swelling, particularly of the face, tongue, or throat. If experiencing these symptoms, seek medical attention immediately. Anaphylaxis, a severe allergic reaction, presents as difficulty breathing or swelling in the throat and demands urgent care.
Some individuals report headaches and dizziness. If these symptoms persist, consulting a healthcare provider is advisable to rule out other potential causes or complications.
Azithromycin can also affect heart rhythm. It is crucial to inform your doctor of any existing heart conditions or medications that may interact adversely. Regular monitoring can help manage any risks associated with this side effect.
In rare cases, the medication may lead to liver problems. Symptoms such as jaundice, dark urine, or persistent nausea necessitate immediate medical evaluation.
Maintaining open communication with your healthcare professional about any side effects experienced throughout treatment is essential for ensuring safety and effectiveness. Adjustments to dosage or alternative therapies might be necessary based on individual reactions.
Comparison with Other HIV Prophylactic Options
Azithromycin shows promise as a prophylactic option for HIV, particularly in specific populations at high risk. Its advantages include ease of administration and relatively mild side effects compared to other treatments.
In contrast, pre-exposure prophylaxis (PrEP) featuring tenofovir and emtricitabine often serves as the gold standard for HIV prevention. PrEP is highly effective, reducing the risk of HIV transmission by over 90% when taken consistently. However, adherence can be a challenge, and it typically requires regular medical follow-ups.
Post-exposure prophylaxis (PEP), which combines antiretroviral medications taken after potential HIV exposure, differs from azithromycin. PEP must be initiated within 72 hours of exposure and taken for 28 days, making it less practical than preemptive treatments like azithromycin for ongoing risk populations.
Another option is the use of long-acting injectable antiretrovirals, such as cabotegravir, which offers a bi-monthly or quarterly administration schedule. This method significantly enhances adherence for some individuals but requires clinical visits, whereas azithromycin can be taken orally and may involve less frequent healthcare interactions.
Studying azithromycin’s role alongside these established treatments provides insights into its potential benefits and optimal use cases. While not a replacement for comprehensive HIV prevention strategies, it can complement existing methods for select groups.
Indications and Patient Selection for Azithromycin Prophylaxis
Azithromycin prophylaxis is indicated for HIV-positive individuals with low CD4 cell counts, specifically those below 200 cells/mm³. Patients with a history of recurrent bacterial infections or those residing in regions with high rates of infections such as pneumonia should also be considered.
Individuals with a history of opportunistic infections drastically benefit from prophylactic measures. Assessing patients for specific risk factors, such as smoking, substance abuse, or poor nutrition, can further refine the selection process. Patients undergoing certain therapies that suppress the immune system may additionally require azithromycin as a preventive strategy.
To ensure proper patient selection, it is essential to evaluate the patient’s overall health status, including any existing comorbidities. Close monitoring for potential drug interactions is necessary, especially for patients on antiretroviral therapy. Implementing regular follow-up appointments can assist in adjusting prophylactic measures based on the patient’s evolving health status.
Education on adherence to azithromycin regimens plays a significant role in achieving desired outcomes. Providing clear guidance and ensuring open lines of communication can facilitate better patient understanding and compliance. Screening for adherence barriers, including socioeconomic factors, will aid in tailoring a supportive approach.
Future Research Directions in Azithromycin and HIV Prevention
Further investigations should focus on optimizing dosages of azithromycin for HIV prophylaxis. Clinical trials can evaluate the impact of varying dosages on HIV transmission rates among high-risk populations. This approach may identify the most effective regimen.
Studies must also explore the long-term effects of azithromycin use in HIV prevention. Research should assess potential resistance patterns that may develop with prolonged use. Understanding resistance mechanisms will inform future treatment protocols.
Another key area involves the combination of azithromycin with other preventative strategies. Investigating interactions between azithromycin and PrEP (pre-exposure prophylaxis) drugs could provide insights into synergistic effects that enhance overall efficacy.
Field studies can benefit from assessing azithromycin’s role in diverse geographical locations. Variability in HIV prevalence and local healthcare practices may influence outcomes. Such research can guide tailored interventions that address specific community needs.
Researchers should also examine the impact of azithromycin on co-infections. Identifying how azithromycin affects other sexually transmitted infections (STIs) in the context of HIV prophylaxis can lead to integrated treatment approaches.
- Conduct thorough research on optimal dosages.
- Assess long-term effects and potential resistance.
- Explore combinations with PrEP and other prevention methods.
- Investigate geographical variations in treatment efficacy.
- Examine interactions with co-infections.
Collaborative efforts among researchers, healthcare providers, and communities will drive these initiatives forward, leading to improved strategies for HIV prevention. Continuous review and adaptation of current practices based on research findings will enhance outcomes for individuals at risk.